Osteochondrosis of the neck is a degenerative disease that literally involves "premature aging", "wear and tear" of the discs, joints and vertebrae in the cervical spine.
Some facts about the disease:
- Osteochondrosis of the neck occurs roughly equally in men and women.
- Most of the time, people between the ages of 30 and 60 get sick.
- As a rule, pathology occurs in people who have to constantly be in one position at work and make monotonous movements.
- The cervical spine has some structural features that allow the disease to have many different manifestations.

Which features of the cervical spine cause the symptoms of osteochondrosis?
- There are holes in the lateral processes of the vertebrae - through them the carotid arteries go right and left through them, which supply the brain with blood.
- The first part of the spinal cord runs through the neck region - it contains fibers that transport nerve impulses to all parts of the body, ensuring movement and sensitivity. When the spinal cord is compressed in the neck, neurological disorders occur throughout the body.
- This part of the spine is very flexible and predisposed to osteochondrosis (although in most cases the disease still develops in the lumbar spine - it is not only highly mobile, it also experiences the greatest stress).
- In the neck area, nerve roots emerge from the intervertebral foramen and form the cervical and brachial plexus. They are responsible for movements in the muscles of the neck, arms, shoulder girdle, skin sensitivity and the regulation of autonomic functions.
- The first vertebra does not have a massive anterior part - a body - it's a bony ring that is placed on a tooth - a bony outgrowth on the second vertebra. Thanks to this, it is possible to turn the head to the side.
Neck pain, headache, weakness, numbness in the hands - symptoms that should force you to see a neurologist. Examination by a specialist and examination using modern equipment will help understand the causes of the pathology and take the most effective measures.
What happens to the vertebrae in cervical osteochondrosis?
The obscure medical term "degenerative process" refers to the following pathological changes in the cervical spine:
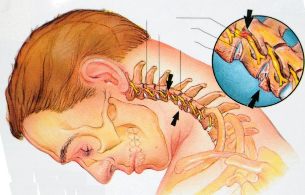
- First of all, the lesion in osteochondrosis covers the intervertebral discs. They become thinner, reducing the distance between adjacent vertebrae. Small cracks, micro-cracks are formed in their outer part. This can lead to a herniated disc over time.
- Damaged intervertebral discs disturb the stability of the vertebral connection.
- You suffer from osteochondrosis of the cervical spine and the intervertebral joints - spondyloarthrosis develops. It also helps compress the nerve roots.
- The pathological process extends to the vertebrae themselves. Due to the fact that the functions of the intervertebral discs are disturbed, the load on them increases. The spine tries to compensate for this injury, bone outgrowths - osteophytes - appear on it.
Treatment of osteochondrosis of the cervical spine
During an exacerbation of osteochondrosis of the cervical vertebra, traction is used (the patient is placed on a bed with a raised headboard and the head is fixed with a special loop) to relieve the intervertebral discs. You need to wear a shants collar for the same purpose. Pain relievers and anti-inflammatory drugs are prescribed to relieve pain. For severe pain that does not go away, the doctor may block: inject an anesthetic solution into the area of the affected nerve roots. Physiotherapy is used: treatment with ultrasound, electrophoresis with novocaine.
When the exacerbation subsides, treatment for cervical spine osteochondrosis includes massage, physical therapy exercises, and physical therapy.
One of the main signs of cervical osteochondrosis is neck pain. Many people who are confronted with this symptom do not go to the doctor and prefer to treat "chondrosis" at home. There are at least two good reasons to refuse self-medication and consult a specialist.
First, painkillers and folk methods do not solve the main problem, although for a while they help to relieve pain. Pathological changes in the spine continue to increase. Over time, this threatens with more serious consequences. To the point that surgery may be required.
Second, neck pain isn't unique to osteochondrosis. There are many other reasons. Only a doctor can understand and prescribe the right treatment.
What symptoms of osteochondrosis of the cervical spine should force you to see a doctor?
The main symptom of cervical osteochondrosis is pain. It can appear in different places, depending on the level at which the pathological process is localized: in the neck, in the shoulder girdle, in the hand, in the area of the heart. Pain is boring by nature, it can burn and be painful.
Other manifestations of the disease:
- Headache, dizziness, flies in front of the eyes, noise, ringing in the ears.
- weakness in the muscles of the neck, shoulder girdle and arms.
- Disorder of skin sensitivity.
- Shoulder and shoulder blade periarthritis: aching neck pain that extends to the arm, difficulty in abduction of the arm over 90 °, weakness and atrophy of the shoulder girdle muscles.
- shoulder-hand syndrome: pain in the shoulder and hand, swelling and stiffness of the fingers, weakness and atrophy of the hand muscles.
- vertebral artery syndrome. Bony growths appear on the vertebrae that squeeze the nerves, as a result of which a reflex spasm of the vertebral artery occurs, which is involved in the blood supply to the brain. Symptoms of cervical osteochondrosis are accompanied by constant headaches that start from the back of the head, spread to the temples, crown, nausea, head noises, ringing in the ears and the flickering of bright spots in front of the eyes.
- Anterior scale muscle syndrome. On the neck are the anterior and middle scalene muscles - they lie next to each other, and between them there is a small space where nerves and blood vessels run. With osteochondrosis of the cervical spine, the anterior scalene muscle becomes tense and squeezes, causing symptoms such as pain on the inner surface of the forearm, shoulder, and fingers. Sometimes the pain radiates to the back of the head. The skin of the hand can become cold, pale, and numb.
- epicondylitis syndrome. In the lower part of the shoulder, on the sides of the elbow joint, there are bony protrusions - the epicondyle. With epicondylitis syndrome caused by cervical osteochondrosis, there are painful sensations that increase when you press. Other symptoms also appear: neck pain, pain when pressing certain points in the cervical vertebrae.
When two parts of the spine are affected at the same time and there is cervicothoracic osteochondrosis, symptoms may appear between the shoulder blades in the area of the heart.
With osteochondrosis, the risk of intervertebral hernia and stroke increases. If you experience the symptoms listed above, contact your doctor.
It is better not to self-medicate. Even if you have tried and tested methods that usually help you manage pain, that doesn't mean you're getting it right.
Pain can be caused not only by osteochondrosis, but also by intervertebral hernias, muscle disorders (myofascial pain syndrome) and as a symptom of other diseases. In order to properly treat the disease, you need to understand its causes and conduct differential diagnosis. This is only possible in a clinic.
In order to identify the cause of the disease and correctly treat the symptoms of cervical osteochondrosis, you need to visit a neurologist and undergo an examination.
At the center of cervical osteochondrosis is the defeat of the intervertebral discs. Their chemical composition is violated, first they swell, then they decrease, cracks and cracks appear in their outer part, they become denser. Then the degenerative process spreads to the vertebrae and intervertebral joints. Due to a decrease in the height of the intervertebral disc, the load on the vertebrae increases, and bone growth appears on them - osteophytes.
What are the causes of osteochondrosis of the cervical spine?
There is no consensus on the causes of cervical osteochondrosis. Different conditions are believed to cause disease. There are different considerations:
- Age-related changes in the spine. Almost all people over 40 have changes in their skeleton, but not everyone has osteochondrosis.
- Neck injuries. Often among the causes of the disease, trauma is indicated: neck contusion, compression fracture, subluxation of the vertebrae. Chronic injuries, such as during intense exercise for athletes, persistent awkward curving postures, and repeated whiplash injuries in motorists, can be of concern.
- Congenital anomalies of the vertebrae: cervical ribs, fusion of adjacent vertebrae, fusion of the first vertebra with the occipital bone, etc.
- Profession. More often, the disease affects people who work in a monotonous posture and constantly perform the same type of movement.
- Interruption of blood supply to the spine, venous insufficiency, edema in the area of the nerve roots.
- Autoimmune diseases.Conditions in which the immune system is not working properly attack the body's own connective tissue and ligaments.
Visit a neurologist. A skilled doctor will understand the root cause of your health problems and will prescribe the correct treatment.
Causes of the exacerbation of cervical osteochondrosis
Osteochondrosis takes the form of alternating exacerbations and periods of improvement when symptoms stop bothering for a while. A further deterioration can be triggered for the following reasons:
- Cumbersome, jerky neck movement.
- Long stay in a monotonous, uncomfortable position. For example, after long periods of work at the computer and after sleeping on an uncomfortable pillow, the neck may start to hurt.
- Stress, nervous strain. With chronic stress, cramps occur in the neck muscles, which can lead to another exacerbation.
- Various diseases, exacerbations of chronic diseases.
- hypothermia. Because of this, many people experience exacerbations in the fall.
- Wrong self-medication with illiterate people. For example, massage and therapeutic exercises are useful during remission, but contraindicated during an exacerbation.
What diseases can have similar manifestations?
Very often the manifestations of "osteochondrosis" are actually associated with a completely different disease. For example, the reason may be hidden in the muscles - there is a condition like myofascial pain syndrome. The pain is caused by the constant tension in the same muscles.
Sometimes the manifestation of "cervical osteochondrosis" is viewed as dizziness associated with otolithiasis - a condition in which crystals of calcium salts build up in the inner ear.
Pain and crunch in the neck, headache - when these symptoms occur, many people "diagnose" osteochondrosis. Everything is clear - if it hurts, you need to take painkillers or do a ukolchik, apply heat, and everything will pass. Why go to the doctor when you can handle it yourself?
However, self-medication often does not lead to anything good. Over time, attacks of pain can become more frequent, stronger, and longer. If you take uncontrolled pain relievers almost every day, you may experience stomach or kidney problems. After all, every medicine has side effects.
And the cause of the pain is not always the root cause of osteochondrosis. To find out the real cause and understand how to deal with it effectively, you need to consult a doctor and undergo an examination.
How does a neurologist diagnose cervical osteochondrosis? What happens in the doctor's office during the examination?
During your first visit, the neurologist will ask you a few questions:
- How long have you had headaches and neck pain?
- Where does the pain occur? What kind of character are they: stab, pain, shoot, pull?
- When does pain usually occur? What is it provoking? What do you feel better after?
- Have you already seen a doctor? Have you been examined and treated? Which one? How long?
- What other symptoms are you bothering about?
- What other chronic diseases do you have?
- Have you recently had a neck injury?
The doctor will then do a neurological exam that will check your reflexes, skin sensitivity, muscle strength and tone. You are asked to turn around, tilt your head to one side, forward and backward. The doctor will give light pressure to specific areas on the neck of your head to determine if pain is occurring.
After the examination, you will be diagnosed and the necessary diagnostic methods will be prescribed.
What diagnostic methods are used in osteochondrosis of the cervical spine?
Testing for cervical osteochondrosis usually includes the following diagnostic methods:
- X-ray of the cervical spine.
- According to the indications, X-ray contrast studies are prescribed: myelography (introduction of contrast into the space around the spinal cord), discography (introduction of contrast into the intervertebral disc), angiography (introduction of contrast into the vessels).
- Computed tomography.
- magnetic resonance imaging.
- If you have severe neurological disorders, you may be prescribed electroneuromyography - a study that determines the passage of electrical impulses in nerves and muscles.
Often, manifestations of cervical osteochondrosis resemble angina pectoris. If after the examination the doctor still has doubts about the diagnosis, you will be prescribed an EKG and other diagnostic methods.





































